Department of Radiation Oncology’s Radiochemistry Division has two primary areas of research, which are apparent from the laboratory names, Radionuclide Production Laboratory and Molecular Radiotherapy Research Laboratory.
The Radionuclide Production Laboratory has the primary objective of producing therapeutic and theranostic radionuclides. The Molecular Radiotherapy Research Lab’s primary objective is to advance the field of molecular radiotherapy for the treatment of cancer. Researchers in the two laboratories collaborate with other investigators at UW, Fred Hutch, and other U.S. academic and government institutions, to develop new theranostic radionuclides and new molecular radiotherapy agents for better cancer therapies. Cancers of the blood and metastatic cancers particularly can benefit from systemically delivered molecular radiotherapy using a highly potent injectable radiopharmaceutical to reach parts of the body that would be difficult or impossible to treat with other types of radiation. These molecular radiotherapy agents are designed to selectively target radiation to blood and cancer cells so that one day they can diminish or eliminate the need for more toxic treatments, such as total body irradiation. Theranostic radionuclides provide opportunities for accurate dosimetric analyses, improved treatment planning and response monitoring.


One of the Radionuclide Production Research Lab’s primary programs involves production of therapeutic and theranostic radionuclides for US investigators. Our research lab
Through a team effort, capitalizing on the capabilities of the UW Medical Cyclotron Facility and the expertise of personnel running that facility, our research lab has developed and optimized a method for producing astatine-211 in quantities required for clinical use. We are also working on producing other radionuclides, termed theranostic radionuclides, that by themselves or in combination with another radionuclide can both treat cancers and be used to image cancers Such theranostic radionuclides or theranostic radionuclide pairs; (1) can be used to determine if a radionuclide therapy will be effective prior to initiating the cancer treatment, (2) can be used for treatment and (3) can also be used to determine the effectiveness of the treatment process. Collaborations are being conducted with researchers at other universities (University of Missouri, Virginia Commonwealth University) and U.S. national laboratories (Brookhaven, Oak Ridge and Los Alamos National Laboratories) for producing radionuclides. Examples of theranostic radionuclides that have been prepared are high specific activity rhenium-186 and tin-117m. We also have on-going R&D efforts on the production of strontium-85, terbium-155 and the radionuclide generator systems selenium-72/arsenic-72 and uranium-230/thorium-226. Radionuclide generators can be obtained when a longer-lived radionuclide decays to a medically-useful short-lived radionuclide, making it possible to use the short-lived radionuclides at locations distant from where they are produced.
Development of new reagents for molecular radiotherapy involves investigation of methods for coupling therapeutic and theranostic radionuclides with biomolecules that target cancer cells to prepare radiopharmaceuticals. Our preclinical studies evaluate methods for radiolabeling cancer targeting biomolecules to provide radiolabeled agents with high in vivo stability and optimal cancer targeting in animal models. We currently have multiple ongoing preclinical studies with investigators at UW and Fred Hutch. Although our lab’s focus is on preclinical radiochemical and radiopharmaceutical studies, we collaborate closely with research partners to translate the work into clinical studies. These studies are in the areas of hematopoietic cell transplantation, which is used in treatment of lymphoma, leukemia and multiple myeloma, and hepatocellular carcinoma. In an extension of the preclinical studies, our lab has served as the radiopharmaceutical production core for clinical trials evaluating At-211 labeled monoclonal antibodies as a method for augmenting conditioning regimes for hematopoietic stem cell transplantation.
Radionuclides are produced by particle irradiation of isotopes of selected elements. During the irradiation process a large amount of heat is generated by the irradiating particle beam impinging on the target material. Durable cyclotron targets are essential for achieving large-scale radionuclide production for preclinical and clinical applications. Efficient heat transfer is a key to developing durable cyclotron targets capable of withstanding a high current of accelerated charged particle beam. We currently have ongoing research projects focused on the development of durable cyclotron targets for producing large quantities of At-211, Tb-155 and Sn-117m.
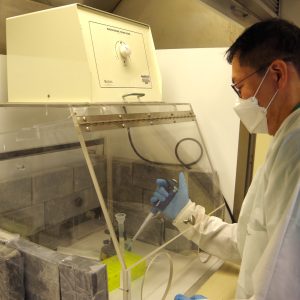
The radionuclide produced must be isolated from the target material before it can be used for labeling of biomolecules. Thus, our radionuclide production research also focuses on the development of highly efficient methods for the isolation of the therapeutic and theranostic radionuclides of interest, and on the establishment of routine production processes. For some radionuclides, like Sn-117m and Re-186, isotopically enriched target materials are required to achieve high production rates and high radioisotopic purity. Further, methods that enable recycling of highly-enriched isotope target materials are critical for reducing the overall cost of those radionuclides. Automation is being studied for improving the radionuclide isolation process. Automation of the isolation process can reduce personnel radiation exposure and increase batch to batch consistency. Importantly, the use of an automated system can alleviate the need for highly trained radiochemists to perform the manual isolation process. For short-lived radionuclides like At-211, there can be an advantage, or even a requirement, to produce and process the irradiated targets near the facility where the activity will be used for preclinical or clinical studies.
A large portion of the research in the Molecular Radiotherapy Research Lab is directed at the use of At-211-labeled monoclonal antibodies in hematopoietic cell transplantation (HCT). We have had long-term collaborations with a number of investigators at the Fred Hutch Cancer Center, including Dr. Rainer Storb, Dr. Brenda Sandmaier, Dr. Oliver Press (deceased), Dr. Damian Green, Dr. Johnnie Orozco and Dr. Roland Walters. We continue to have ongoing collaborative clinical and preclinical research projects with Fred Hutch investigators. In those collaborations the goal is to determine if the use of highly potent radiation from At-211-labeled antibodies can lead to new conditioning regimens that are more effective and less toxic than the conventional conditioning regimens, which use high intensity chemotherapy and total body irradiation to kill cancer cells and suppress immune response. HCT can be used in the treatment of cancers such as lymphoma, leukemia and multiple myeloma, and can also be used for treating nonmalignant blood disorders.
Liver cancer (hepatocellular cancer, or HCC) is the third-most lethal cancer globally, responsible for over 830,000 deaths in 2020. The 5-year survival rate is less than 20% for all stages and only 2% for advanced stages, highlighting the need to develop new agents for early detection and better therapy regimens for this disease. Collaborations with Professor James Park, in the UW Department of Surgery, have demonstrated high selectivity for targeting HCC in an animal model. In those studies, we found that coupling the positron-emitting radionuclide zirconium-89 to a monoclonal antibody that targets the cell surface proteoglycan glypican-3, expressed on over 80% of liver cancers, can detect HCC tumors with both high sensitivity and accuracy in vivo. The same antibody, when coupled to therapeutic radionuclides, such as yittrium-90 and thorium-227, effectively suppresses and even halts the growth of the tumor. Research effort to further develop this theranostic approach for liver cancer diagnosis and treatment is ongoing.